Molar pregnancy or also known as Hydatidiform mole, and is one of the causes of miscarriages, although it is a rare disorder, it can bring complications if it is not detected or treated in time. In this article, I am going to give you the most crucial information regarding hydatidiform mole, and I am going to include ultrasound images as well.
What is molar pregnancy?
Molar pregnancy is characterized by the abnormal growth of trophoblasts, the cells that normally develop into the placenta.
There are two types of molar: Complete and partial molar pregnancy.
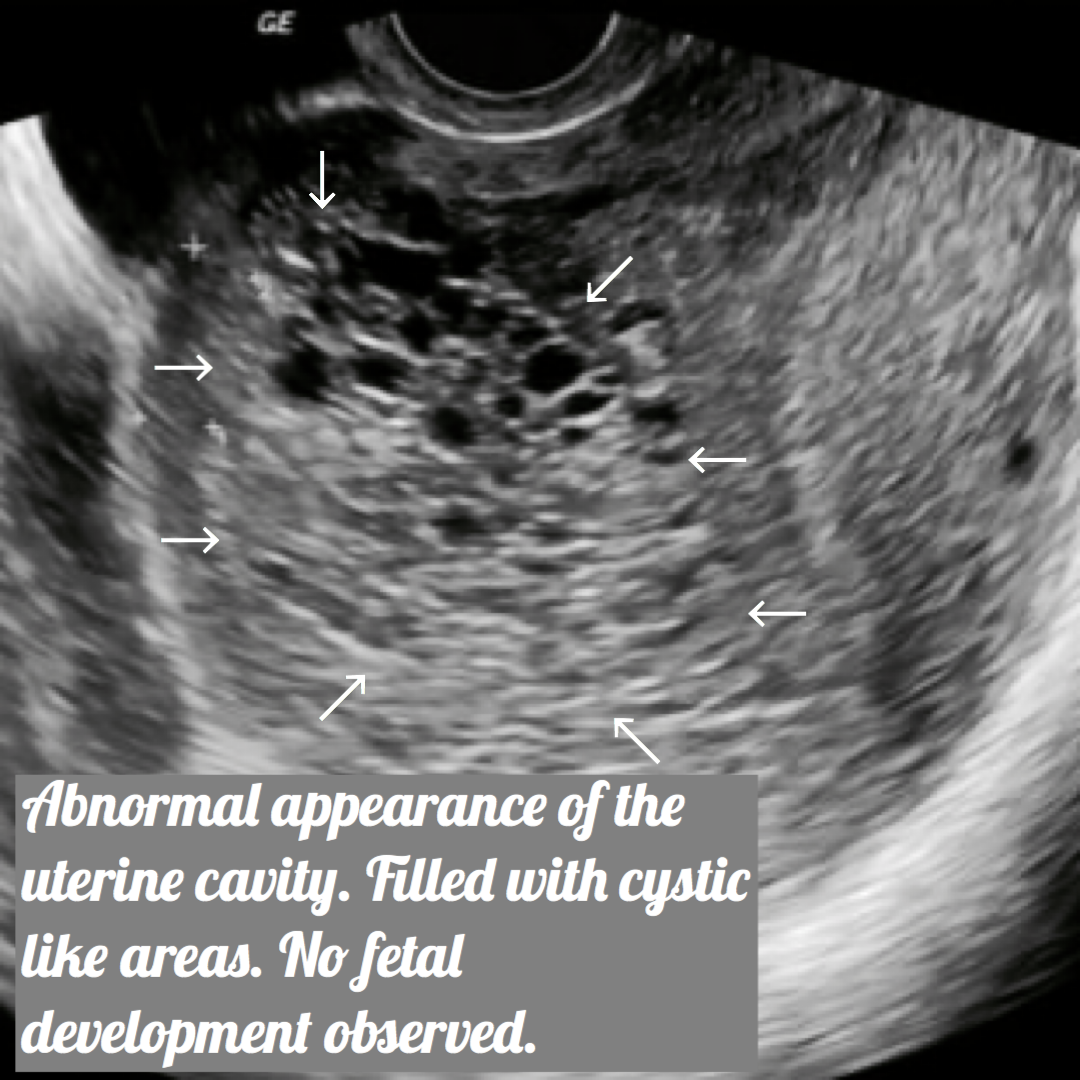
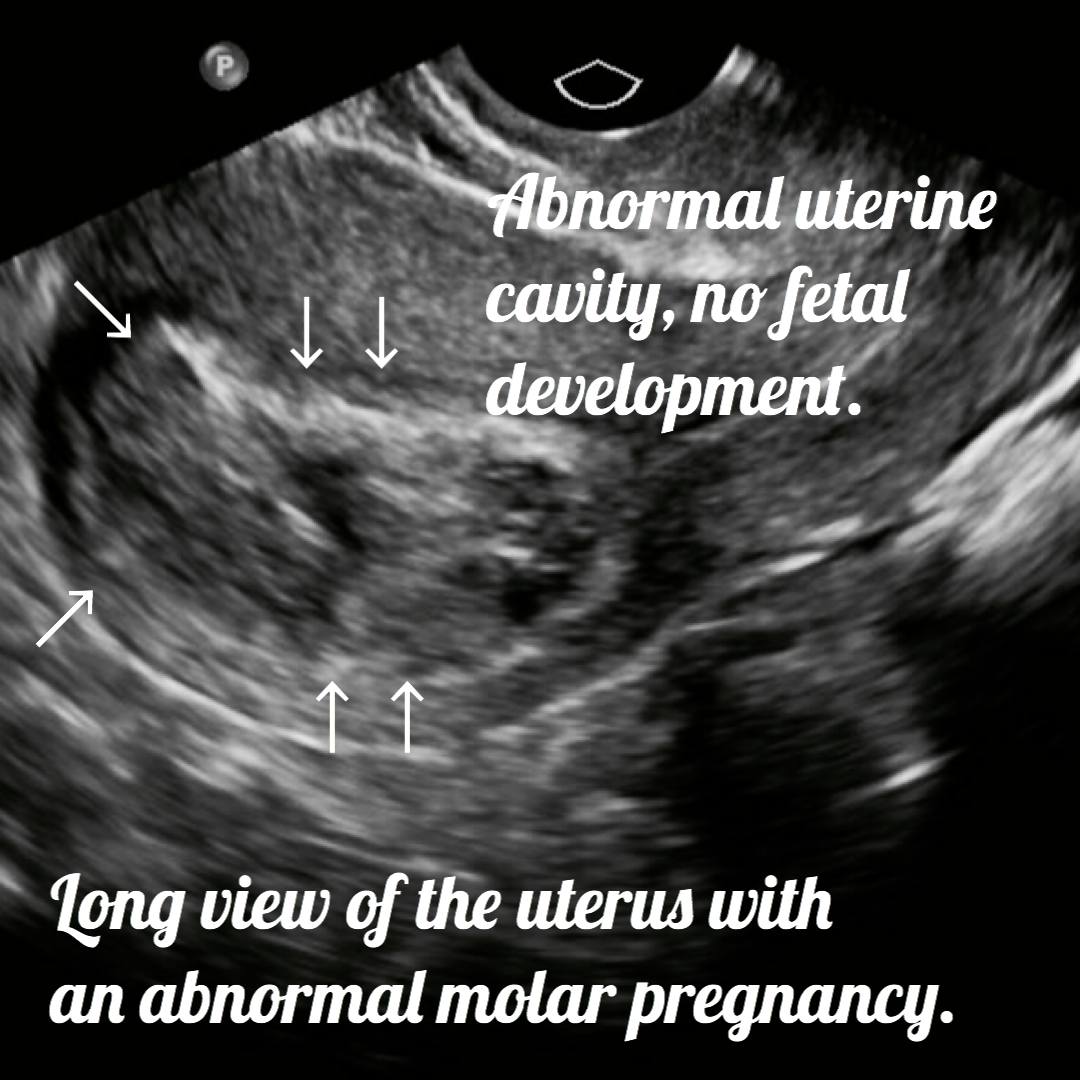
- Complete molar pregnancy: The placental tissue is abnormal and swollen and appears to form multiple fluid-filled cysts all over the uterine cavity, with the absence of a fetus.
- Partial molar pregnancy: There may be healthy placental tissue along with abnormally forming placental tissue as well. There may also be the formation of a fetus, but the fetus is not able to survive and is usually miscarried early in the pregnancy.
As I mentioned earlier, in the molar pregnancy, the trophoblast, or the tissue that forms the placenta, is abnormal, swollen, and contains cysts. If we recapitulate a little about the function of the placenta, we already know that the role of the placenta is vital for the healthy development of a baby. Therefore, if the placenta doesn’t develop normally, inevitably a baby can’t survive.
Related post: Everything about the placenta. Ultrasound images included.
A molar pregnancy can have serious complications; these complications might include a rare form of cancer. We are talking about this, more in deep below. Therefore, it requires early treatment.
Molar pregnancy symptoms.
The molar pregnancy usually begins as a healthy pregnancy, in which the first-trimester pregnancy symptoms take place. However, there are specific symptoms that should be discussed with your doctor as soon as they appear.
Related post: Pregnancy symptoms for the first trimester.
Among the specific symptoms of mole, we have:
- Severe nausea and vomiting.
- Dark vaginal abnormal bleeding.
- Pelvic discomfort, pressure, and sometimes severe pain.
- Vaginal passage of grape like cysts and tissue.
How to know if you have any risk for molar pregnancy?
Unfortunately, 1 in 1,000 cases of pregnancies is diagnosed as a hydatidiform mole.
Among the most common risk factors are:
- Maternal age: If you are under 20, or over 35 years of age, the risks of having a molar pregnancy are higher.
- History of molar pregnancy: 1 in 100 cases of molar are recurrent. This means that, if you have had a molar pregnancy before, you are at a higher risk of having another molar pregnancy.
What are the causes of molar pregnancy?
A molar pregnancy is nothing more and nothing less than an abnormal fertilized egg. During regular fertilization, the maternal egg contains 23 chromosomes, and the father’s sperm provides 23 additional chromosomes. When the genetic material of the egg and the sperm joins, an egg with 46 chromosomes is now fertilized to create a healthy baby.
Complete molar pregnancy: An egg without the normal chromosomes is fertilized by one or two sperm, and all of the genetic material is from the father. In this situation, the chromosomes from the mother’s egg are lost or inactivated, and the father’s chromosomes are duplicated.
Partial or incomplete molar pregnancy: In this case, the mother’s chromosomes are good, but the father provides abnormally two sets of chromosomes instead of only one. As a result, the embryo has 69 chromosomes (3 sets of chromosomes) instead of 46. This most often occurs when two sperm fertilize one single egg, resulting in an extra copy of the father’s genetic material.
Share the post!
Prevention.
A molar can’t be 100% prevented. The fertilization process occurs, and we can only hope for the best. Anyway, there are always measures that you can implement to carry a normal pregnancy, or to detect early if there is a molar pregnancy.
Those measurements might include:
- If you had a history of molar pregnancy, talk to your doctor before trying to conceive.
- If you had a previous molar pregnancy, wait at least six months to 1 year to get pregnant again. After this time, your chances of having another molar are significantly lower.
- Take control of your body and health even before you get pregnant if you are trying to conceive.
- Track your periods, so you can notice when you get pregnant right away.
- Your first prenatal appointment is crucial and is the beginning of different tests, including early ultrasounds, to ensure the viability and normal development of the baby.
- If you start having abnormal symptoms, talk to your doctor as soon as possible.
- Know your options, and discuss with your doctor about prenatal genetic testing.
Ultrasound images of molar pregnancy.

Treatment.
A molar can’t develop a healthy viable pregnancy. To prevent further complications, the abnormal placental tissue must be removed. Treatment usually consists of one or more of the following steps:
- Dilation and curettage (D&C). To treat a molar, your doctor will remove the molar tissue from your uterus with a procedure called dilation and curettage (D&C). A D&C is usually done as an outpatient procedure in a hospital.
- Hysterectomy. Rarely, if there is an increased risk of gestational trophoblastic neoplasia and there’s no desire for future pregnancies, the uterus may be removed (hysterectomy).
- HCG monitoring. After the molar tissue is removed, your doctor will repeat measurements of your HCG level until it returns to normal. If you continue to have HCG in your blood, you may need additional treatment. Once treatment for the molar pregnancy is complete, your doctor may continue to monitor your HCG levels for six months to one year to make sure there’s no remaining molar tissue.
Complications.
After a molar has been removed with the D and C, molar tissue may rarely remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). Unfortunately, this can occurs in approximately 15 percent of complete molar pregnancies and up to 5 percent of partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG), a pregnancy hormone after the molar pregnancy has been removed. In some cases, an invasive hydatidiform mole penetrates deep into the muscle layers of the uterine wall, which can cause abnormal vaginal bleeding.
The good news is that persistent GTN can nearly always be successfully treated, most often with chemotherapy. Another treatment option is removal of the uterus or hysterectomy, if there is no desire for future pregnancies.
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. A complete molar pregnancy is more likely to have this complication than a partial molar.
Early treatment is the key to treat molar pregnancy successfully, and almost 100% of the cases are cured.
Final words.
As you can see, molar pregnancies are an uncommon and very frightening complication of pregnancy. And obviously, a stressful experience to overcome when you are trying to grow a family. Fortunately, with the advances in science today, the likelihood of complications is low if the treatment was effective.
Before trying to conceive, it is advisable always to do a general check-up with your doctor to rule out any problems in advance, and once you are pregnant, start with your routine check-ups to monitor the development of a healthy pregnancy early.
I hope this information has been helpful to you, as usual, thanks for reading this post. Don’t forget to share your thoughts with us.
Zadi, xo.
Disclaimer: The medical information on this post is for educational and entertainment use only. Under no circumstances, this information is to replace your doctor’s advice or to treat any disease. For proper care, always visit your doctor.










I?e learn some just right stuff here. Certainly price bookmarking for revisiting. I wonder how much attempt you put to make this sort of magnificent informative web site.
Thanks.
Thank you. Very helpful
Thanks Jessica
[…] Molar pregnancy information. Ultrasound included. […]
[…] Molar pregnancy information. Ultrasound included. […]
I had a complete molar pregnancy that was removed with D&C in January of 2021. Fortunately, I did not have any complications or need further treatment afterward. I did, of course, have the weekly hcg blood draws for several months, but I was blessed that my numbers went down as they should and stayed down. My complete molar pregnancy story can be read here: https://www.mamarissa.com/my-complete-molar-pregnancy-story-pregnant-with-a-tumor/
It is such a strange situation to be in and most people have no idea what molar pregnancy is. Thank you for putting this information out there. It can be hard to find accurate information on this topic when you are suddenly hit with the unexpected news of a molar pregnancy.
Wow Marissa your story is truly remarkable. I thank you for sharing it with me and our readers. You were extremely lucky to had a molar pregnancy for 16 weeks and still be fine afterwards. Molar pregnancy is a serious condition but can be very manejable if you find it early. That’s why I recommend having a first ultrasound at 7 weeks to make sure that a fetal pole is growing. Let’s keep in touch dear.