Endometrial hyperplasia occurs in approximately 133 out of every 100,000 women per year. The majority of cases occur after menopause among women from 50 to 55 years of age. On the other hand, atypical endometrial hyperplasia is mostly reported in women between 60 and 64 years of age. It is known that in many cases, endometrial hyperplasia, especially atypical endometrial hyperplasia, can develop endometrial cancer, hence the importance of making an early diagnosis and a proper treatment. In this post, we’ll go over everything you need to know about endometrial hyperplasia. As usual, you’ll see ultrasound images of endometrial hyperplasia. Ready? Let’s begin.
What is endometrial hyperplasia?
The uterus is formed by the myometrium, which is the muscular or outer layer of the uterus, and the endometrium, also known as the lining, which is the innermost layer of the uterus. Inside this cavity (endometrium) is where a pregnancy implants, develops and grows.
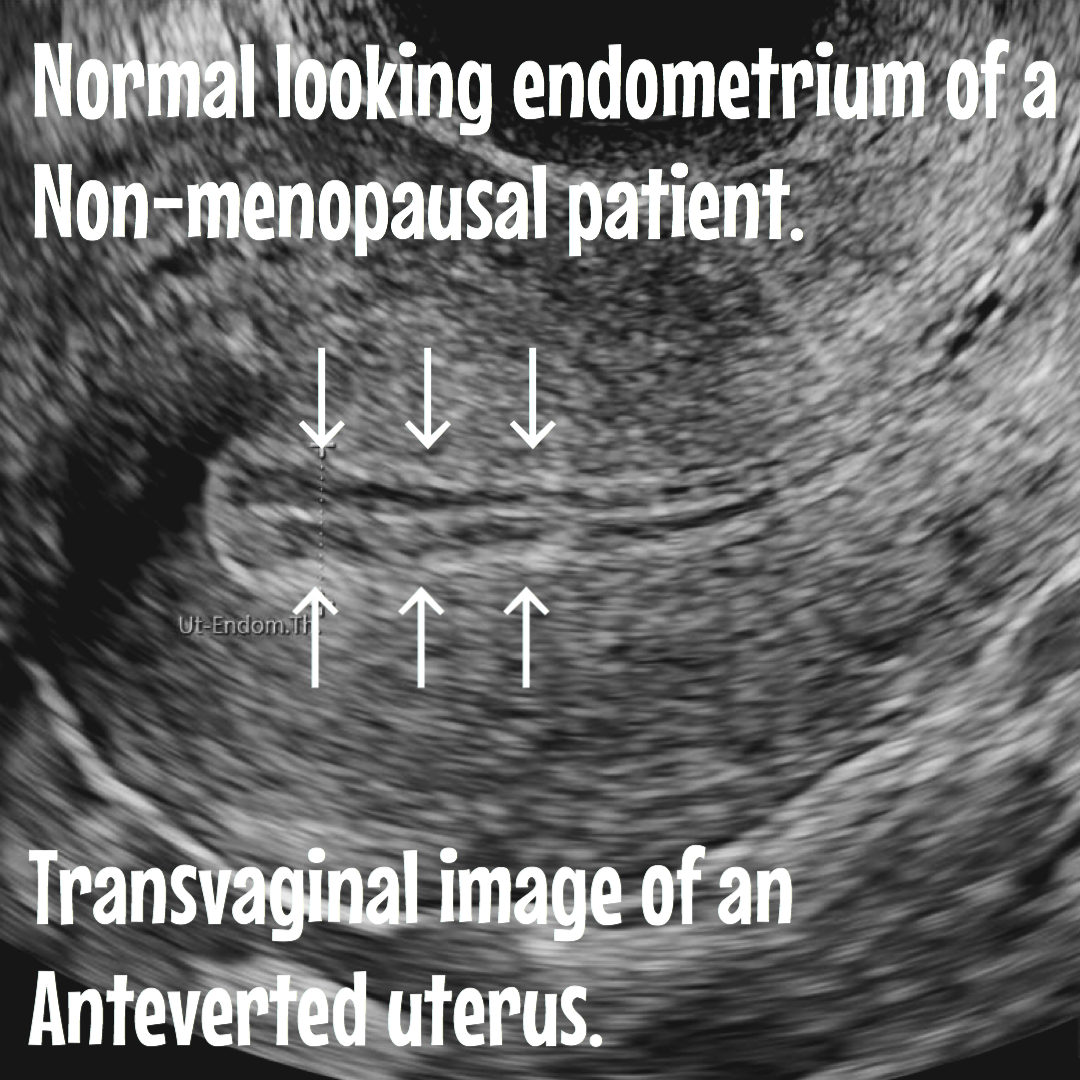
In reproductive age, the endometrium fluctuates in size and appearance, depending on hormones and the menstrual cycle. A thinner endometrium is seeing right after the period, and naturally gets thickened as it approaches to the second week of the period, all the way until the next menstrual period.
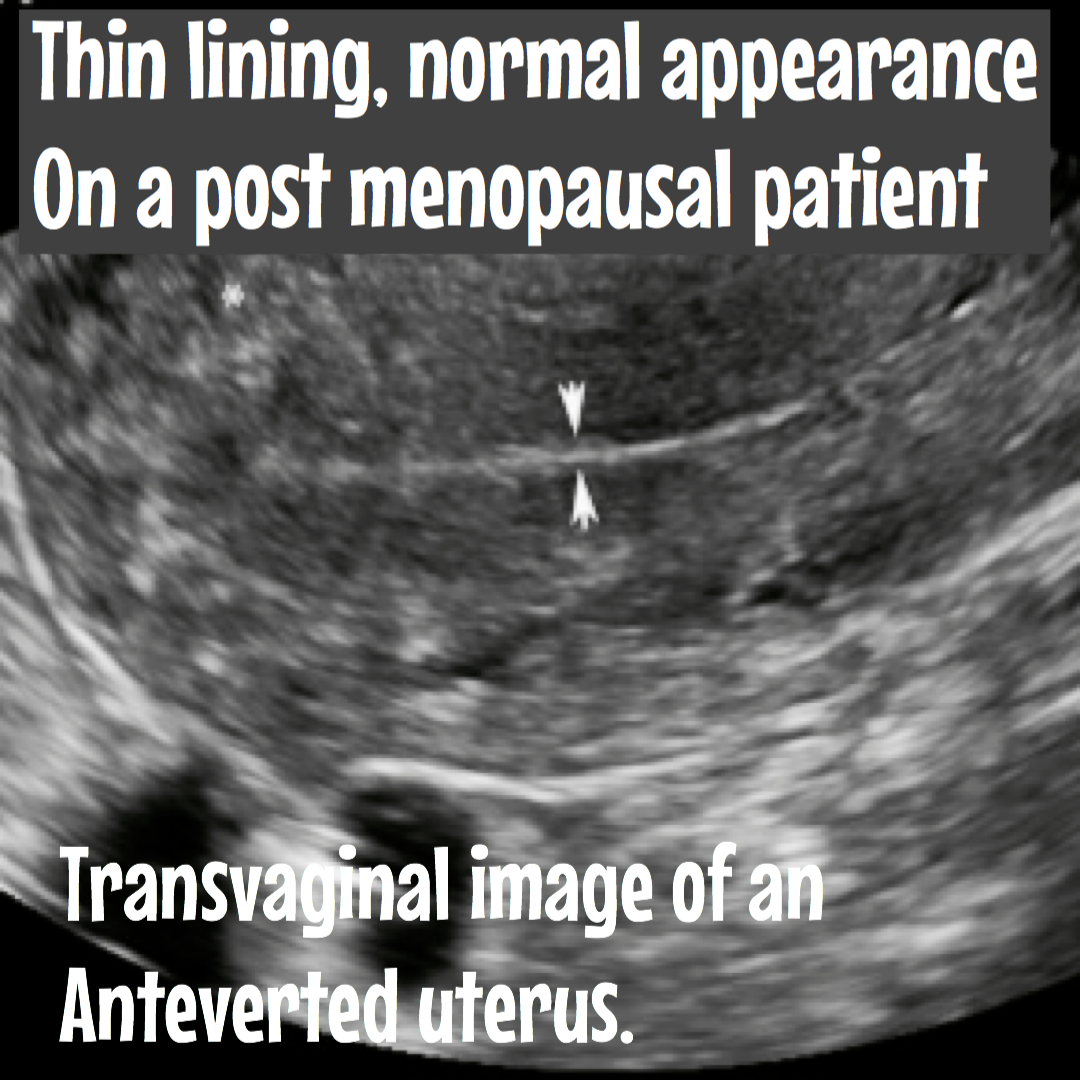
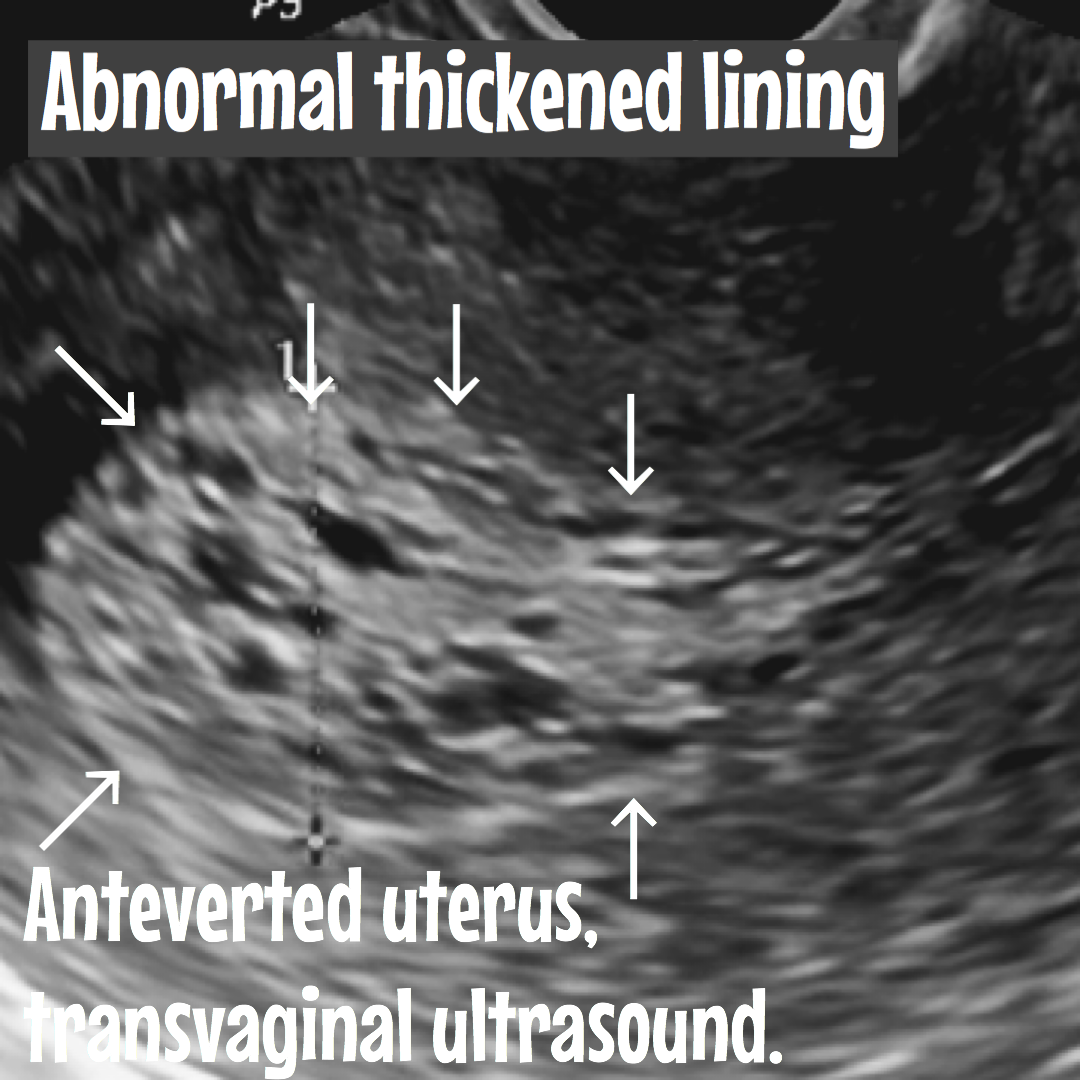
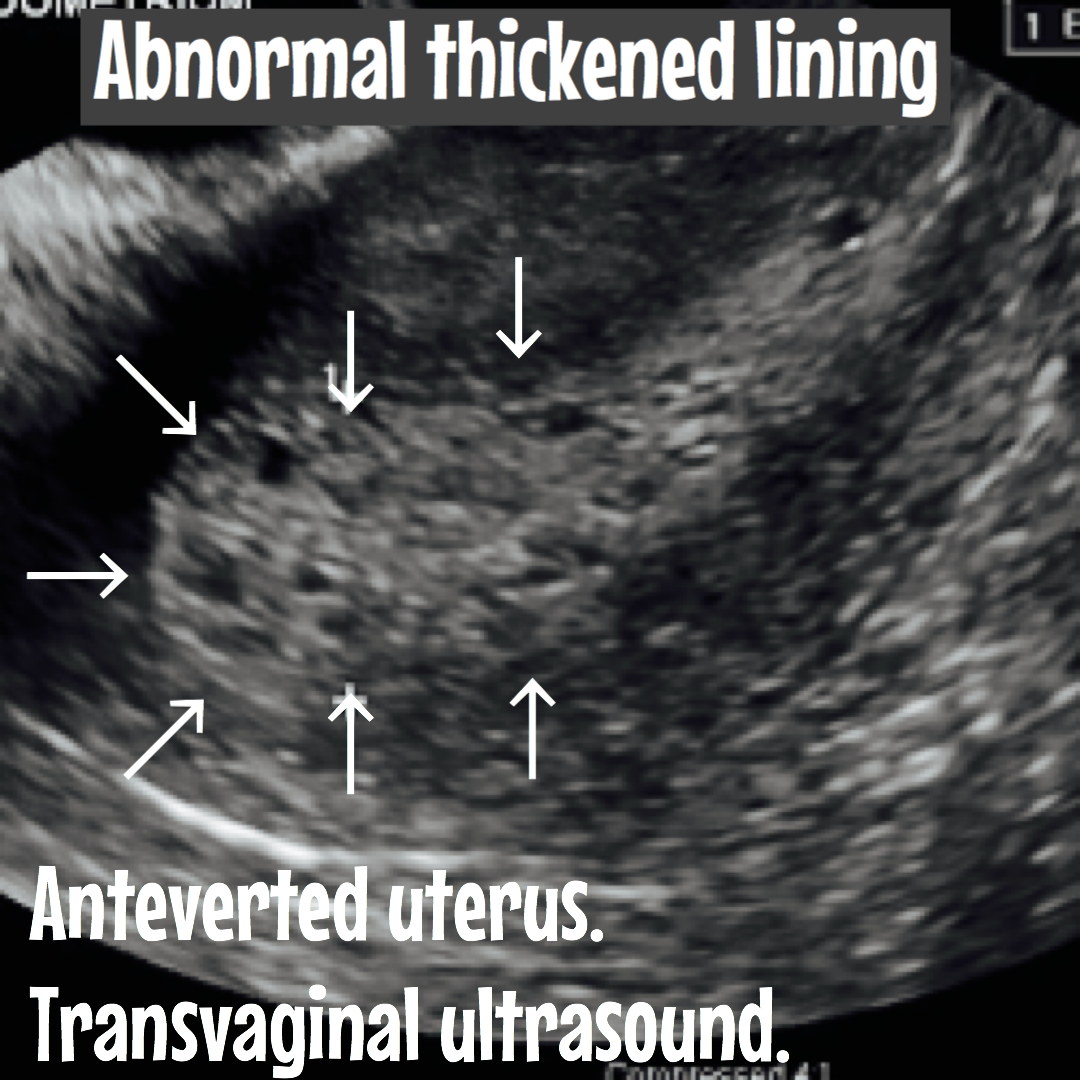
Once the woman reaches menopause, the ovaries stop producing hormones and ovulating, the menstrual cycle ends, and therefore the endometrial cavity should not get thickened anymore. The normal measurements of an endometrium in postmenopausal patients are 5 mm or 0.5 cm or less. If it is larger than this size, it is thickened.
Causes of endometrial hyperplasia.
The excess of estrogen causes endometrial hyperplasia without any progesterone. If ovulation does not occur, progesterone is not made, and the lining is not shed with the menstrual cycle. The endometrium may continue to grow in response to the excess of estrogen. The cells that make up the lining may crowd together and may become abnormal. This condition, called hyperplasia, may lead to cancer in some women.
Risk factors in developing endometrial hyperplasia.
- Polycystic ovarian syndrome or PCOS.
- Obesity.
- Nulliparity (No pregnancies).
- Lynch syndrome (hereditary nonpolyposis colorectal cancer) is associated with a 22%–50% lifetime risk of developing into endometrial cancer.
- Early menarche (Getting menstrual periods at an early age).
- Late menopause.
- Personal history of certain conditions, such as diabetes mellitus, or thyroid disease.
- Cigarette smoking.
- Family history of ovarian, colon, or uterine cancer.
Classification of endometrial hyperplasia:
Endometrial hyperplasia is classified in relation to the type of glandular stromal changes, that are described as simple or complex. Is also classified based on the presence or absence of atypia (irregular or abnormal cells) in the endometrial cavity.
This results in four categories:
- Simple without atypia
- Complex without atypia
- Simple with atypia
- Complex with atypia
Simple represents a mild increase in gland number.
Complex has an increase in gland-to-stroma ratio greater than 50% with cellular disorganization. Cells usually show mitosis.
Atypical appearance is represented by nuclear enlargement, abnormal chromatin, and polymorphism of the lining cells.
Most common signs and symptoms of endometrial hyperplasia.
Endometrial hyperplasia can occur at any stage in a woman’s life.
In young women can be produced by the presence of pre-existing conditions such as
Diabetes, thyroids problems, lynch syndrome, PCOS, obesity etc.
After menopause, it is produced by an increase in the production of estrogen, without the presence of progesterone, which can be the result of taking medications such as Tamoxifen (A medication for Breast cancer patients) or any other hormones etc.
Either way, the most frequent symptom of patients with endometrial hyperplasia is:
Abnormal uterine bleeding.
- Menorrhagia: Increased vaginal bleeding, greater than 80 ml or bleeding that lasts longer than eight days.
- Menometrorrhagia: Increased irregular bleeding (thought of as a mix of menorrhagia and metrorrhagia)
- Postmenopausal bleeding: Any amount of vaginal bleeding, including spotting or staining after a woman had already experienced a cease in menstruation due to menopause.
How is the diagnosis of endometrial hyperplasia made?
The American Congress of Obstetricians and Gynecologists recommends that any women over the age of 35 experiencing abnormal uterine bleeding symptoms should be given a test to rule out endometrial hyperplasia.
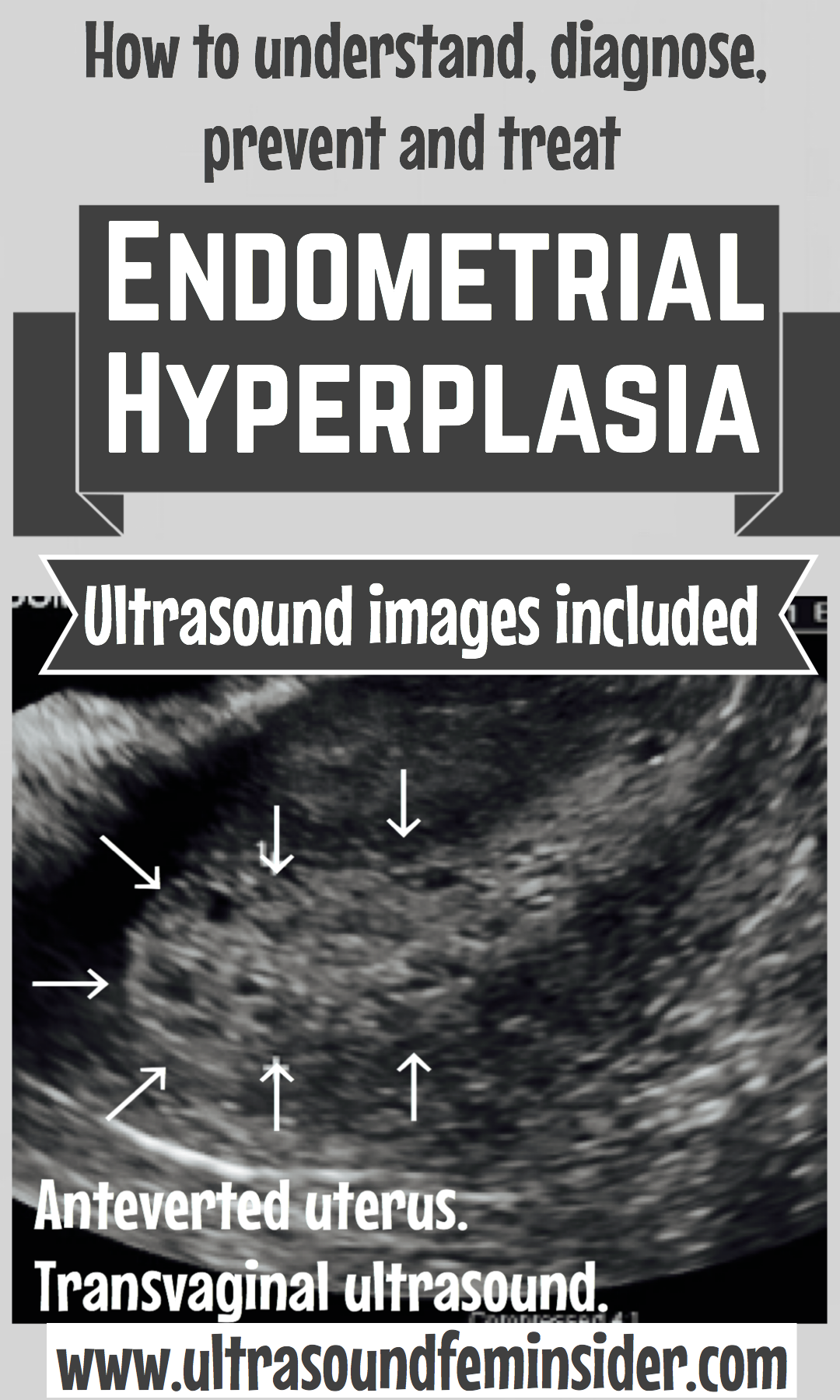
The first examination consists of a vaginal ultrasound to assess the appearance and size of the endometrium and/or any other potential causes.
If the endometrium is reported as thickened, an endometrial biopsy can be performed. Other biopsy methods can be performed in the operating room, including dilation and curettage (commonly referred to as D&C) and hysteroscopy.
How an ultrasound looks like if there is endometrial hyperplasia present?
Treatment for endometrial hyperplasia.
Endometrial hyperplasia treatments can be varied and are according to the specific situation of each patient.
In reproductive age, endometrial hyperplasia can cause infertility; therefore, the recommended treatment is progestin therapy. There are also other methods, such as Intrauterine hormonal devices (IUD’s) or oral contraceptive pills.
Related post: All about IUD or Intrauterine device.
For postmenopausal patients, who have already finished having a family, and fertility is not a problem, hormonal therapies can be tried, but if there are no improvements, or there is a possibility of developing endometrial cancer, in this case the hysterectomy will be the most recommendable treatment.
The most important thing you should know is that, if you have abnormal bleeding, you should be evaluated by a gynecologist to find the causes, and implement an appropriate treatment specifically for you.
Sharing is caring!!
Prevention for endometrial hyperplasia.
As you may have already realized, endometrial hyperplasia is mostly caused by a hormonal imbalance in the absence of other pre-existing medical conditions. Therefore there are some changes in lifestyle that can significantly improve your hormones and your menstrual cycle. Among these changes are:
- Maintain a healthy weight and body mass.
- Healthy diet.
- Regular physical exercise.
- Drink plenty of water, avoid sugars.
If there are pre-existing conditions like thyroid problems or PCOS. You must treat these diseases correctly to stabilize the hormones.
Natural remedies for endometrial hyperplasia.
- Vitamin D: A deficiency in vitamin D may lead to low energy, body and joint pains, thyroid problems, and depression. Therefore, normal values of vitamin D will regulate hormones and prevent endometrial hyperplasia. The primary recommended source of Vitamin D is the sunlight and also by taking a supplement.
- Sleep: Lack of sleep can have a negative impact on hormones and can create the hormone levels of a pre-diabetic. Aim for 8 hours of quality, uninterrupted sleep per night.
- Omega-3 Fatty Acids: Omega-3 essential fatty acids play a crucial role in producing hormones; therefore, they are highly beneficial in balancing them. In the list of healthy foods that are rich in Omega-3 fatty acids you have: flax and chia seeds, red kidney and navy beans, almonds and broccoli.
- Sandalwood Essential Oil: The powerful fragrance of sandalwood essential oil triggers peaceful feelings and results in the overall reduction of emotional stress, which, over time, can lead to hormone imbalances.
- Magnesium: Magnesium is also required to treat all hormonal imbalance issues including PCOS (polycystic ovary syndrome), PMS (premenstrual dysphoric disorder), perimenopause (The beginning of the process where a woman transition into menopause), thyroid conditions, adrenal fatigue, and anxiety. Also, it helps in the production of the thyroid hormone, hence, preventing thyroid disease. The best source of magnesium is from magnesium-rich foods, including tamarinds, soybeans, navy beans, red kidney beans, spinach, kale, chickpeas, lentils, figs, prunes, or artichokes.
Related posts:
Final thoughts about Endometrial hyperplasia.
If a woman is diagnosed with endometrial hyperplasia, this is one of the reasons for the development of infertility. Different stages of the disease can lead to the inability to have children, hormonal disorders, and endometrial cancer. Several types of pathology differ in symptomatology and treatment options. The most common is glandular hyperplasia, which causes the proliferation of glandular tissue, accompanied by the appearance of cysts of different sizes within the lining. The most dangerous is the atypical. This one is considered a precancerous condition. Timely diagnosis and treatment is the ideal way to prevent the onset of the disease.
Therefore, Whether you are still in reproductive age, or the menopause stage, visiting a doctor to diagnose endometrial hyperplasia correctly, and receiving proper treatment is paramount to avoid significant problems later on.
I hope this article has been able to help you. Feel free to leave comments below.
Zadi, XO.










[…] Endometrial hyperplasia. Ultrasound included. […]
whoah this blog is fantastic i love reading your posts. Keep up the good work! You know, lots of people are hunting around for this info, you could help them greatly.
Hi there just wanted to give you a quick heads up and let you know a few of the images aren’t loading correctly. I’m not sure why but I think its a linking issue. I’ve tried it in two different browsers and both show the same outcome.