Pregnancy failure is a common problem in the first trimester with failure rates approaching 25%. A threatened abortion is defined as bleeding and cramping in the first 20 weeks of pregnancy. Ultrasound plays a key role in evaluating women with threatened abortion since HCG levels do not always correlate with a specific diagnosis. Unfortunately miscarriages in the first trimester of pregnancy are very common, usually caused by genetic or chromosomal problems. Fortunately, not always that there is an abnormal ultrasound in the first trimester of pregnancy, it necessarily means that a miscarriage is going to occur. In this article I am going to give the most common causes of abnormal first trimester ultrasound. Ultrasounds images are included in this post as well. Ready? Let’s begin.
Sharing is caring!
What are the early signs of an early miscarriage?
If you have any symptoms of a miscarriage, you should contact a doctor right away to have an evaluation. It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage.
The most common signs of a miscarriage are:
- Heavy bleeding, blood that looks read. Keep in mind that light bleeding early in pregnancy is fairly common, and does not mean you will have a miscarriage.
- Brown discharge: This may look like coffee grounds. This “discharge” is actually old blood that has been in the uterus for a while and is just coming out slowly.
- Spotting, bright red bleeding or clots
- Passage of tissue through the vagina
- A gush of clear or pink vaginal fluid
- Abdominal pain or cramping
- Dizziness, lightheadedness, or feeling faint
Most common reasons for an abnormal first trimester baby ultrasound are as follow.
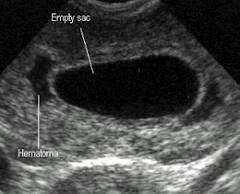
Subchorionic hematoma or bleedings.

Subchorionic hematoma or Subchorionic bleedings Is the most common sonographic abnormality in the presence of a live embryo. Vaginal bleeding affects 25% of all women during the first trimester. In women whose sonogram shows a Subchorionic hematoma, the outcome of the fetus depends on the size of the hematoma, the mother’s age and the fetus gestational age.
If the Subchorionic hematoma appears in the late first or second trimester. The risks for miscarriage, stillbirth, placental abruption or preterm labor are increased.
However small asymptomatic Subchorionic hematoma vs Subchorionic bleeding in the first trimester of pregnancy, associated with no other complications can resolve by itself without any intervention.
Anembryonic pregnancy or Blighted ovum.
A blighted ovum (also known as “anembryonic pregnancy”) happens when a fertilized egg attaches to the uterine cavity, but the embryo does not develop. Cells develop to form the pregnancy sac, but not the embryo itself. A blighted ovum occurs within the first trimester, often before a woman knows she is pregnant. A high level of chromosome abnormalities usually causes a woman’s body to naturally miscarry.
Blighted ovum Is a form of failed pregnancy. Defined as a gestational sac in which the embryo failed to develop. A large gestational sac without the visualized embryo is unequivocal evidence of a failed anembryonic pregnancy.
Embryonic demise and Bradycardia.
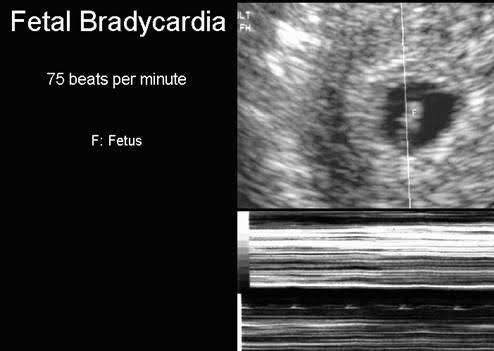
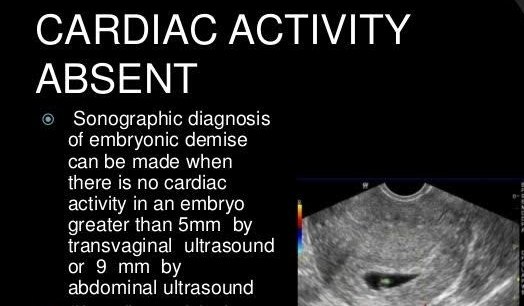
The most convincing evidence that pregnancy has failed is the documentation of embryonic demise. As stated previously, all embryos greater than 5 mm in size should demonstrate cardiac activity. Embryonic bradycardia is a poor prognosticator of pregnancy viability and needs follow up. An embryonic heart rate less than 90 beats per minute, in embryos less than 8 weeks is associated with 80% rate of eventual embryonic demise.
Ectopic pregnancy.
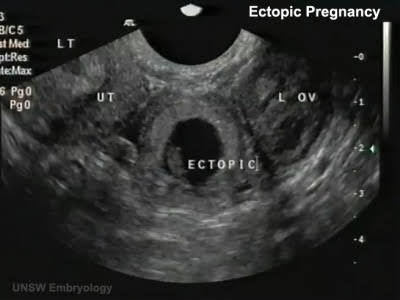
An ectopic pregnancy occurs when a fertilized egg implants and grows outside the main cavity of the uterus. An ectopic pregnancy most often occurs in a fallopian tube, which carries eggs from the ovaries to the uterus. This type of ectopic pregnancy is called a tubal pregnancy. Sometimes, an ectopic pregnancy occurs in other areas of the body, such as the ovary, abdominal cavity or the lower part of the uterus (cervix), which connects to the vagina.
The most reassuring sign that an ectopic pregnancy is not present, is the sonographic demonstration of a normal intrauterine pregnancy. Which means that when the HCG levels are 1500 IU or more an intrauterine pregnancy has to be seen. If not the possibility of an Ectopic pregnancy is really high, Follow up with HCG in blood and Ultrasound are highly recommended.
Patients that are in high risk for ectopic pregnancy have:
- Previous ectopic pregnancy. If you’ve had this type of pregnancy before, you’re more likely to have another.
- Inflammation or infection. Sexually transmitted infections, such as gonorrhea or chlamydia, can cause inflammation in the tubes and other nearby organs, and increase your risk of an ectopic pregnancy. Or previous history of pelvic inflammatory disease ( PID )
- Fertility treatments. Some research suggests that women who have in vitro fertilization (IVF) or similar treatments are more likely to have an ectopic pregnancy. Infertility itself may also raise your risk.
- Tubal surgery. Surgery to correct a closed or damaged fallopian tube can increase the risk of an ectopic pregnancy.
- Choice of birth control. The chance of getting pregnant while using an intrauterine device (IUD) is rare. However, if you do get pregnant with an IUD in place, it’s more likely to be ectopic. Tubal ligation, a permanent method of birth control commonly known as “having your tubes tied,” also raises your risk, if you become pregnant after this procedure.
- Smoking. Cigarette smoking just before you get pregnant can increase the risk of an ectopic pregnancy. The more you smoke, the greater the risk.
Transvaginal ultrasound has an accuracy of 90% in the evaluation for ectopic pregnancy.
The most common adnexal finding is a complex mass which represents hemorrhage. Other adnexal findings included a normal adnexa or a well formed adnexal ring with or without a yolk sac or embryo.

Related posts:
Pregnancy diet. What to eat or what to avoid during pregnancy.
How to get ready for a baby as a new parent.
All you need to know about ectopic pregnancy.
Final thoughts about abnormal first trimester ultrasound.
Having an abnormal first ultrasound is indeed a traumatic experience. On my next article I will be talking about Twin pregnancies, and the following week I will be going week by week on scanning, if you read until the end, thank you so much.
Feel free to comment if you have any questions.
Zadi, xo
Disclaimer: Due to HIPPA compliance and regulations all patient information is protected on this site. Also the information provided on my blog is designed to provide helpful information about the topic and are made with the best of my knowledge, therefore is not intended to diagnose or treat any medical condition, For diagnosis or treatments on any medical problems consult a physician. The author is not responsible or liable for any mistreated pathologies or wrong treatments.










[…] Abnormal first trimester ultrasound. […]