When it comes to preeclampsia an informed decision can be the difference between life and death, this post is not intended to scare you but to create awareness about the importance of receiving prenatal care with the right professionals. This post is going to be all about preeclampsia in pregnancy, a guide about preeclampsia from a medical perspective.
What is the medical definition of preeclampsia in pregnancy?
Pre-eclampsia is a disorder of pregnancy characterized by the onset of high blood pressure and often a significant amount of protein in the urine also known as proteinuria. When arises the condition usually begins after 20 weeks of pregnancy However, in some cases, it occurs earlier, or after delivery. Pre-eclampsia increases the risk of poor outcomes for both the mother and the baby.
Blood pressure is defined as high when it is greater than 140 mmHg systolic or 90 mmHg diastolic at two separate times, more than four hours apart in a woman after twenty weeks of pregnancy. Pre-eclampsia is routinely screened for during prenatal care.
Hypertensive disorders affect five to 10 percent of pregnancies in the United States and can lead to a number of complications, including preterm birth, maternal morbidity and mortality, and long-term risk of maternal cardiovascular disease.
Early identification of pregnant women at risk of developing early-onset preeclampsia is important in order to allow referral for more intensive surveillance or the application of therapies to prevent the condition from becoming more severe. Importantly, the American College of Obstetricians and Gynecologists (ACOG) has found there are no accurate, predictive tests at this time to determine whether a woman will develop preeclampsia and therefore continues to recommend against other methods for predicting preeclampsia. A detailed medical history and routine blood pressure measurements are the best tools available to alert ob-gyns of potential risk.
Sharing is caring.
What causes preeclampsia in pregnancy?
Doctors can’t yet identify one single cause of preeclampsia, but some potential causes are being explored. These include:
Genetic factors:
Blood vessel problems
Autoimmune disorders
There are also risk factors that can increase your chances of developing preeclampsia in pregnancy. These include:
- Preeclampsia is more common in women who are carrying twins, triplets or other multiples.
- Advanced maternal age, over the age of 35.
- Getting pregnant in your early teens.
- First-time pregnancy.
- Obesity.
- Having a history of high blood pressure, diabetes mellitus or kidney disorder.
Having certain conditions before you become pregnant such as chronic high blood pressure, migraines, type 1 or type 2 diabetes, kidney disease, a tendency to develop blood clots, or lupus increases your risk of preeclampsia.
Your risk of preeclampsia is also increased if your baby was conceived with in vitro fertilization.
Early and consistent prenatal care can help your doctor diagnose preeclampsia sooner and avoid complications. Having a diagnosis will allow your doctor to provide you with proper monitoring until your delivery date.
Signs and symptoms of preeclampsia.
When symptoms are present, the most common ones are:
- Persistent headache.
- Swelling in your hands and/or face.
- Sudden weight gain.
- Changes in your vision.
- Pain in the right upper abdomen.
During a physical exam, your doctor may find that your blood pressure is 140/90 mm Hg or higher. Urine and blood tests can also show protein in your urine, abnormal liver enzymes, and low platelet levels.
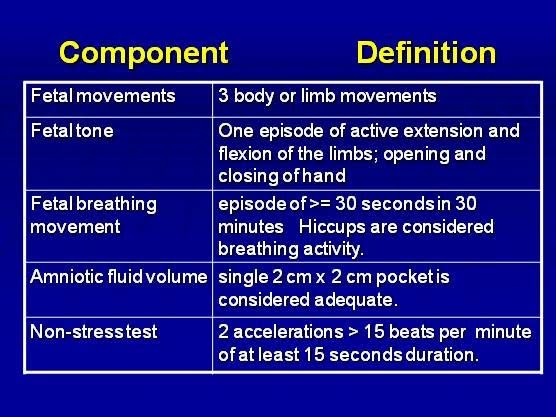
At that point, your doctor may do a nonstress test to monitor the fetus. A nonstress test is a simple exam that measures how the fetal heart rate changes as the fetus moves. An ultrasound may also be done to check your fluid levels and the health of the fetus.
What to know about the complications.
The more severe your preeclampsia and the earlier it occurs in your pregnancy, the greater the risks for you and your baby. Preeclampsia may require induced labor and delivery.
Delivery by cesarean delivery (C-section) may be necessary if there are clinical or obstetric conditions that require a speedy delivery. Otherwise, your doctor may recommend a scheduled vaginal delivery. Your obstetric provider will talk with you about what type of delivery is right for your condition.
Complications of preeclampsia may include:
- Fetal growth restriction: Preeclampsia affects the arteries carrying blood to the placenta. If the placenta doesn’t get enough blood, your baby may receive inadequate blood and oxygen and fewer nutrients. This can lead to slow growth known as fetal growth restriction, low birth weight or preterm birth.
- Preterm birth: If you have preeclampsia with severe features, you may need to be delivered early, to save the life of you and your baby. Prematurity can lead to breathing and other problems for your baby. Your health care provider will help you understand when is the ideal time for your delivery.
- Placental abruption: Preeclampsia increases your risk of placental abruption, a condition in which the placenta separates from the inner wall of your uterus before delivery. Severe abruption can cause heavy bleeding, which can be life-threatening for both you and your baby.
- HELLP syndrome: HELLP which stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count, HELLP syndrome is a more severe form of preeclampsia, and can rapidly become life-threatening for both you and your baby.
- Symptoms of HELLP syndrome include nausea and vomiting, headache, and upper right abdominal pain. HELLP syndrome is particularly dangerous because it represents damage to several organ systems. On occasion, it may develop suddenly, even before high blood pressure is detected or it may develop without any symptoms at all.
What happen when pre-eclampsia is not controlled?
Eclampsia. When preeclampsia isn’t controlled, eclampsia which is essentially preeclampsia plus seizures can develop. It is very difficult to predict which patients will have preeclampsia that is severe enough to result in eclampsia.
Often, there are no symptoms or warning signs to predict eclampsia. Because eclampsia can have serious consequences for both mom and baby, delivery becomes necessary, regardless of how far along the pregnancy is.
Other organ damage. Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on the severity of preeclampsia.
Cardiovascular disease. Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you’ve had preeclampsia more than once or you’ve had a preterm delivery. To minimize this risk, after delivery try to maintain your ideal weight, eat a variety of fruits and vegetables, exercise regularly, and don’t smoke.
What is the treatment for preeclampsia in pregnancy?
In some cases, you may be given medications to help lower your blood pressure. You may also be given medications to prevent seizures, a possible complication of preeclampsia.
Your doctor may want to admit you to the hospital for more thorough monitoring. You might be given intravenous (IV) medications to lower your blood pressure or steroid injections to help your baby’s lungs develop quicker.
Prevention of preeclampsia.
In certain cases you may be able to reduce your risk of preeclampsia with:
Low-dose aspirin. If you meet certain risk factors including a history of preeclampsia, multiple pregnancies, chronic high blood pressure, kidney disease, diabetes or autoimmune disease your doctor may recommend a daily low-dose aspirin (81 milligrams) beginning after 12 weeks of pregnancy.
Calcium supplements. In some populations, women who have calcium deficiency before pregnancy and who don’t get enough calcium during pregnancy through their diets might benefit from calcium supplements to prevent preeclampsia. However, it’s unlikely that women from the United States or other developed countries would have calcium deficiency to the degree that calcium supplements would benefit them.
It’s important that you don’t take any medications, vitamins or supplements without first talking to your doctor.
Before you become pregnant, especially if you’ve had preeclampsia before, it’s a good idea to be as healthy as you can be. Lose weight if you need to, and make sure other conditions, such as diabetes, are well-managed.
Once you’re pregnant, take care of yourself and your baby through early and regular prenatal care. If preeclampsia is detected early, you and your doctor can work together to prevent complications and make the best choices for you and your baby.
Postpartum surveillance: Its necessary to prevent additional morbidity as preeclampsia/eclampsia can develop postpartum.
Risk reduction and successful clinical outcomes require avoidance and management of severe systolic and diastolic hypertension in women with:
Preeclampsia, Eclampsia, Chronic hypertension or superimposed preeclampsia.
Related posts:
Third trimester weeks, the ultimate checklist.
Having a baby on a budget, 9 powerful tips to do it.
What an Ultrasound should include when scanning a patient with Preeclampsia?
- Fetal Biometry/measurements of the baby: to rule out Intrauterine growth restriction(IUGR)
- Heart monitoring: for Viability.
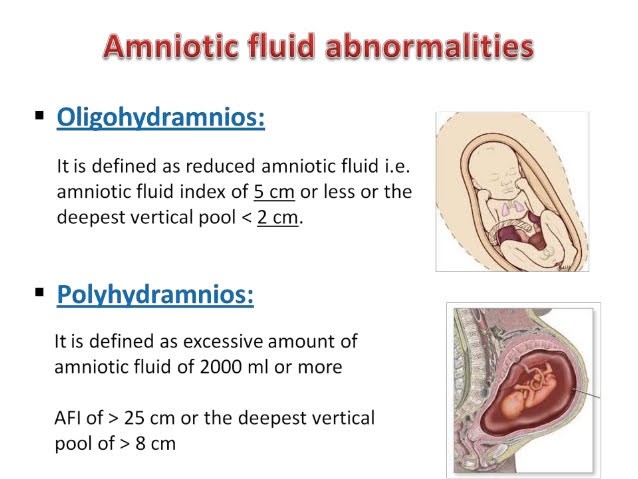
- Amniotic fluid measurements: to rule out OLIGOHYDRAMNIOS or POLYHYDRAMNIOS.
Biophysical profile: To rule fetal distress, Biophysical profile includes fetal movements, fetal tones, fetal breathing, amniotic fluid index, and a Non-stress test to correlate the BPP.
Final thoughts about pre-eclampsia in pregnancy.
During pregnancy, it’s important to keep you and your baby as healthy as possible. This includes eating a healthy diet, taking prenatal vitamins with folic acid, and going for regular prenatal care checkups. If you are diagnosed with preeclampsia your doctor will take care of you, follow his advise and you should be fine.
Zadi, xo.
Disclaimer: Due to HIPPA compliance and regulations all patient information is protected on this site. Also, the information provided on my blog is designated to provide helpful information/education about the topic and are made with the best of my knowledge, therefore, is not intended to diagnose or treat any medical condition, For diagnosis or treatments on any medical problems consult a physician. The author is not responsible or liable for any mistreated pathologies or wrong treatments.











Very instructive and helpful. Thanks for a great review.
Thanks, I am glad you find it helpful
Your post is extremely helpful. I was diagnosed with preeclampsia and I need it to have done guidance.
I am glad to help Denise, thanks.