The First Trimester Screening is an early non-invasive evaluation that combines a maternal blood screening test with an ultrasound evaluation of the fetus to identify risks for specific chromosomal abnormalities, including Down Syndrome Trisomy-21 and Trisomy-18. Intravaginal sonography (US) and quantitative testing of serum levels of human chorionic gonadotropin (HCG) have become the standard testing to establish the presence of normal intrauterine pregnancy (IUP), failed IUP, and ectopic pregnancy during pregnancy, specifically starting in the first trimester. In today’s article I’m going to talk about First trimester abnormal pathologies detected with ultrasound. As usual, ultrasound photos with the explanations are going to be starting in the middle of the post. Ready? Let’s get started.
Sharing is caring!
If you arrived at the end of the first trimester without any complications means that you have a great chance that everything ends well, however there are still many exams that you must do in the time that you wait for the arrival of your baby, so the best thing is to enjoy and try not to worry so much.
Summary of First trimester abnormal ultrasound.
Subchorionic hematoma or Subchorionic bleedings.
Subchorionic bleedings are the most common sonographic abnormality in the presence of a live embryo. Vaginal bleeding affects 25% of all women during the first trimester. In women whose sonogram shows a Subchorionic hematoma, the outcome of the fetus depends on the size of the hematoma, the mother’s age, and the fetus gestational age.
However small asymptomatic Subchorionic hematoma vs Subchorionic bleeding associated with No other complications can resolve by itself.
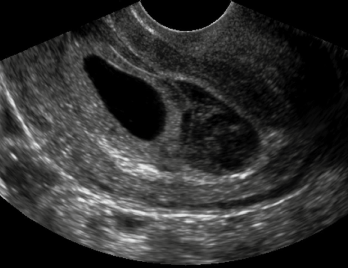
Anembryonic pregnancy (Blighted ovum).
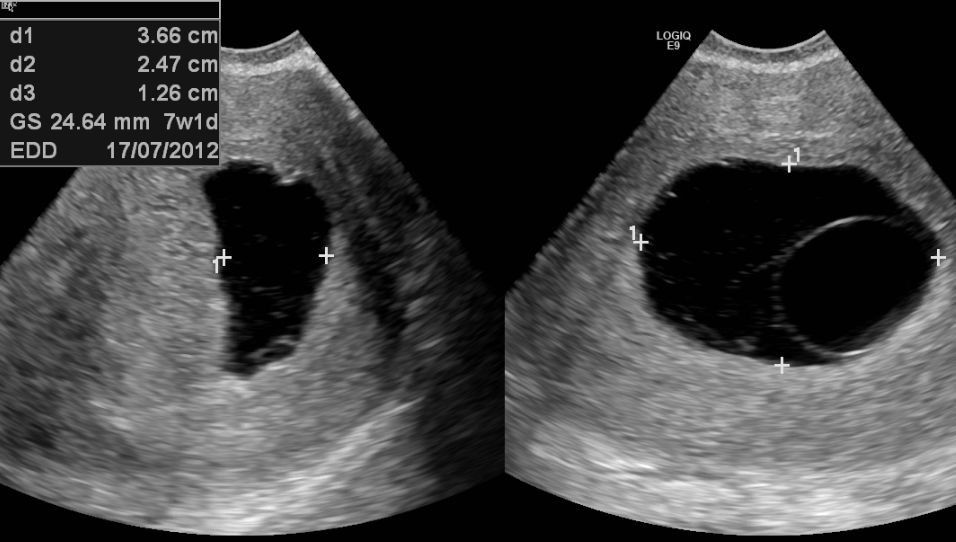
Is a form of failed pregnancy defined as a gestational sac in which the embryo failed to develop. A large gestational sac without the visualized embryo is unequivocal evidence of a failed Anembryonic pregnancy.
Embryonic demise and Bradycardia.
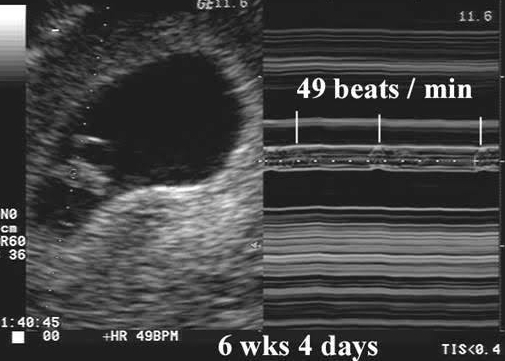
The most convincing evidence that pregnancy has failed is the documentation of embryonic demise. As stated previously, all embryos greater than 5 mm in size should demonstrate cardiac activity. Embryonic bradycardia is a poor prognosticator of pregnancy viability and needs follow up. An embryonic heart rate less than 90 beats per minute, in embryos less than 8 weeks is associated with 80% rate of eventual embryonic demise.
About half of major structural abnormalities can be diagnosed in the first trimester. Increased nuchal translucency appear to be associated with cardiac and skeletal defects and may facilitate early detection, remember nuchal translucency is done at week 11, I have a dedicated post explaining more in detail about that test.
If you are pregnant, and your pregnancy has been so far normal and you are sensitive to Abnormalities, please skip this post. I will link below other normal posts for you.
All about your normal 9 week ultrasound.
All about normal 10 week ultrasound.
First trimester abnormal pathologies detected with ultrasound.
Acrania:
A fetal anomaly characterized by a partial or complete absence of the top portion of the skull, with complete but abnormal development of brain tissue. The condition is frequently associated with Anencephaly and is considered by the medical community as “incompatible with life.” This anomaly appears during the beginning or end of the fourth week of fetal development. The dermatocranium normally becomes the epidermis of the scalp, but in Acrania the dermatocranium remains a membranous coverage. Therefore, the migration of mesenchymal tissue under the calvarium ectoderm does not happen; leading to an absence of the calvarial dermal bones of the skull, related musculature, and dura mater. The brain may still develop, but without the walls of the cranium shaping it, it will not differentiate between the two hemispheres and morph into a single mass that will not be able to sustain life.

Holoprosencephaly (HPE):
Is a cephalic disorder in which the prosencephalon (the forebrain of the embryo) fails to develop into two hemispheres. Normally, the forebrain is formed and the face begins to develop in the fifth and sixth weeks of human pregnancy. The condition can be mild or severe. Most cases are not compatible with life and result in fetal death in utero. When the embryo’s forebrain does not divide to form bilateral cerebral hemispheres (the left and right halves of the brain), it causes defects in the development of the face and in brain structure and function.
In less severe cases, babies are born with normal or near-normal brain development and facial deformities that may affect the eyes, nose, and upper lip.
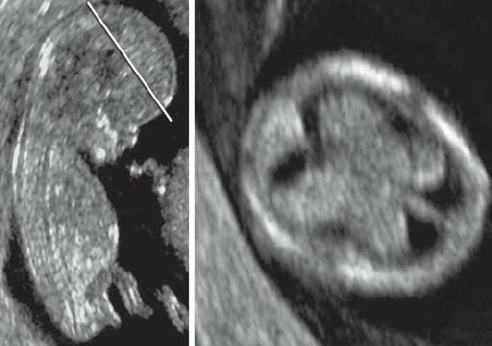
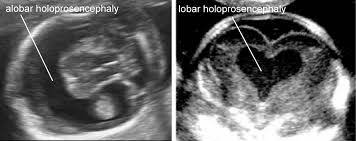
Even though this condition can be seen since the first trimester is not until the Anatomy ultrasound when is diagnosed at 18 weeks, and that’s due to the size of the baby’s head.
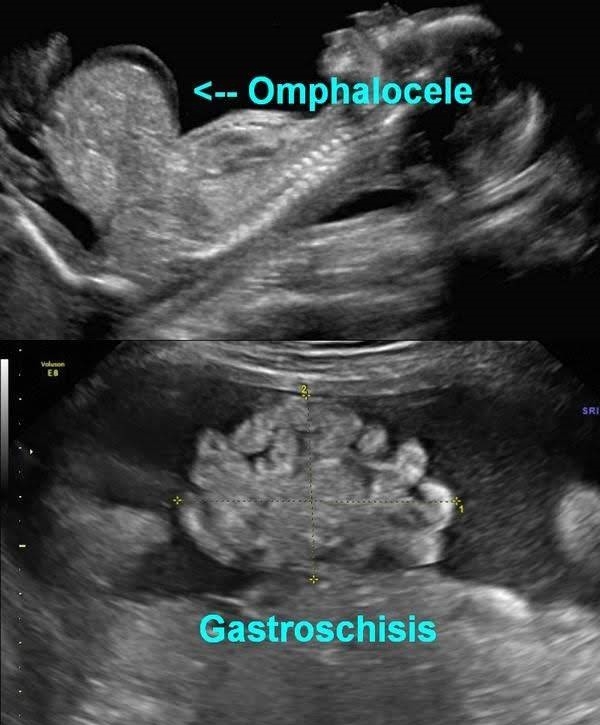
Omphalocele:
Is a birth defect of the abdominal wall. The infant’s intestines, liver, or other organs stick outside of the belly through the belly button. The organs are covered in a thin, nearly transparent sac that hardly ever is open or broken. As the baby develops during weeks six through ten of pregnancy, the intestines get longer and push out from the belly into the umbilical cord. By the eleventh week of pregnancy, the intestines normally go back into the abdominal cavity. If this process fails to happen, then more specific testing has to be done for the diagnosis.
Gastroschisis:
Is an abdominal wall defect to the side of the umbilical cord. The infant is born with intestines protruding through the defect and no protective sac is present. Gastroschisis is rarely associated with other birth defects. Gastroschisis is a life-threatening event requiring immediate intervention.
Hydrops fetalis: Is a serious condition of the fetus or newborn. It is a condition where abnormal amounts of fluid build up in two or more body areas causing swelling. Severe swelling can interfere with how the body organs work and often results in death of the infant shortly before or after delivery.


Final thoughts about First trimester abnormal pathologies detected with ultrasound.
I know that having an abnormal first trimester ultrasound is not a good experience for parents. However, based on the results the pathology can be properly treated for the best outcome for mom and baby. I hope this article helps and good luck.
Zadi, XO
Disclaimer: The information provided on my blog is designed to provide helpful information about the topic and are made with the best of my knowledge. Therefore, is not intended to diagnose or treat any medical condition, For diagnosis or treatments on any medical problems consult a physician. The author is not responsible or liable for any mistreated pathologies or wrong treatments.










Congrats on pregnancy. Check out our blog for moms and moms to be and join our community and conversations. Would love to hear your thoughts and advice you can share with other ladies. Comment on some of our various topics we have up and under older posts ??
I definitely will
Thanks
I also really appreciate if you follow me back thanks
We have many topics we would love ur insight and advice on
A very informative blog.
Thanks Robyn , I am so glad you like it
I went through 3 stillbirths from hydrops, wish I knew then what I know now!
Everyone (and myself) assume that they will have a healthy pregnancy. I did for my first born. My second pregnancy could not have been anymore different. A diagnosis of cystic hygroma changed my world forever
I understand exactly why you are saying dear, unfortunately pregnancy is a long process and anything can change at any time, I am going to post about abnormalities later on, I am not sure exactly when , and cystic hygroma is one of the topics
That is great, awareness is everything. I had never heard of it before. Feel free to visit my blog, I am sharing my pregnancy journey after a cystic hygroma diagnosis
I will definitely visit and follow your blog dear, know that you are indeed not alone, and I know your pain, you have an angel that has to go back very quickly but I am sure you will have a beautiful family one day !!! ??
Would you talk more on these points?
It’s best to take part in a contest for top-of-the-line blogs on the web. I will recommend this web site!